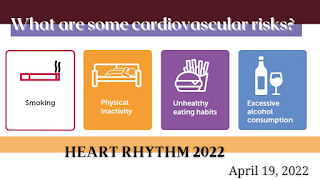
What are some cardiovascular risks?
Risk factors for heart disease: high blood pressure, high cholesterol, and
smoking. Some risk factors for heart disease cannot be
controlled, such as your age or family history. But you can take steps to lower
your risk by changing the factors you can control. The
importance of resting heart rate (HR) as a prognostic factor and potential
therapeutic target is not yet generally accepted. Recent large epidemiologic
studies have confirmed earlier studies that showed resting HR to be an
independent predictor of cardiovascular and all-cause mortality in men and
women with and without diagnosed cardiovascular disease. Clinical trial data
suggest that HR reduction itself is an important mechanism of benefit of
beta-blockers and other heart-rate lowering drugs used after acute myocardial
infarction, in chronic heart failure, and instable angina pectoris.
Pathophysiological studies indicate that a relatively high HR has direct
detrimental effects on the progression of coronary atherosclerosis, on the
occurrence of myocardial ischemia and ventricular arrhythmias, and on left
ventricular function. Studies have found a continuous increase in risk with HR
above 60 beats/min. Although it may be difficult to define an optimal HR for a
given individual, it seems desirable to maintain resting HR substantially below
the traditionally defined tachycardia threshold of 90 or 100 beats/min.
Depression is a risk factor for both onset of cardiovascular disease
(CVD) and increased morbidity and mortality for those with CVD. Many, but not
all studies, have found that depressed patients have alterations in heart rate
(HR) and heart rate variability (HRV). This variability is thought to reflect
autonomic dysfunction. HR tends to be higher in depressed patients and HRV
lower. Both higher heart rates and lower HRV increase CVD risk. Beta-blockers
reduce HR and increase HRV and should be considered for depressed patients with
CVD, elevated HR and/or reduced HRV. Exercise has similar, but smaller effects.
Few studies have examined the effects of psychological interventions on HRV and
the results have either been modest or examined only short term. Future
research should focus on well-characterized subgroups of depressed patients at
risk for CVD with assessment of other important factors that may affect HRV and
CVD risk. Studies of high frequency HRV need to account for the effects of
respiration.
High blood pressure (BP), cigarette smoking, diabetes mellitus, and
lipid abnormalities are major modifiable risk factors for cardiovascular
disease (CVD). Among these, high BP is associated with the strongest evidence
for causation and has a high prevalence of exposure. However, there is
considerable evidence that a biologically normal level of BP in humans is
considerably lower than what has been traditionally employed in clinical
practice and research, leading to an underrepresentation of the role that BP
plays as a risk factor for CVD. We propose the following integrated theory for
CVD causation that is supported by a robust body of coherent and consistent
evidence: CVD in humans is primarily caused by a right-sided shift in the
distribution of BP.


Comments
Post a Comment